Indigenous peoples experience in Australia. Three times more sight loss than non-Indigenous peoplemaking a relationship Space for perspective.
Much of that is attributable to diabetic macular edema (DMO). Here, the blood vessels behind the attention (the retina) are damaged by high blood sugar. Over time, it Causes swelling (edema) of the central part of the retina (macula)..
Macular edema blurs central vision, reducing people's ability to acknowledge faces, drive and work, and perform other essential tasks. DMO is influenced around 23,000 Indigenous people in AustraliaMost of them are of working age. Similar trends have been reported with indigenous populations in other developed states, including New Zealand, Canada And United States.
The excellent news is that DMO is treatable, with known medications. Anti-VEGF agents. We did a world first. Clinical trial To test a long-acting DMO treatment for Indigenous Australians. In doing so, we also learned about conducting culturally sensitive country research.
Long-lasting treatment
When injected into the attention by an ophthalmologist (eye surgeon), anti-VEGF drugs are secure and effective for treating DMO. The injection is painless, as the attention is anesthetized. The catch is that anti-VEGF agents are relatively short-acting, requiring them to be reapplied as often as every month.
Many Indigenous patients find it complex and impractical to participate for a wide range of reasons. Ten to 12 eye appointments a year. So another is required.
Long-acting medications can be found. An example is the dexamethasone implant (known commercially as Ozurdex(R)), a steroid injected into the attention. The dexamethasone implant only must be dosed every three months.
The dexamethasone implant is PBS approved for DMO in Australia but has never been evaluated in an indigenous population. This is significant because a possible side effect of steroid medications is increased pressure in the attention. If left untreated, this could result in a condition that’s influenced by steroids. Glaucoma.
It is considered glaucoma. Less commonly among natives, suggesting differences in eye pressure physiology between Caucasian and native eyes. Additionally, the incidence of steroid-induced subtype glaucoma has never been studied in indigenous populations. This is particularly vital for people far-off, as glaucoma is a “silent disease”, requiring regular check-ups to detect and treat.
gave Historical barriers that prevent this type of research. Cultural and geographic aspects include a scarcity of endorsement by local health services and “staff champions”.
The creator provides.
Not just what to research, but how
I Lions Eye InstituteTry to beat these obstacles with us The OASIS Study – World's first clinical trial in ophthalmology to recruit exclusively indigenous patients.
We structured our study around ten key aspects for fulfillment including access to Aboriginal medical services for all participants, free and secure treatment, free transport, appointment reminders, and cultural safety training for all trial staff. Included. Wherever possible, study visits were made inside the patients' usual Aboriginal medical service. Study participants may include friends, family and staff members. This helped with communication and a way of security and trust.
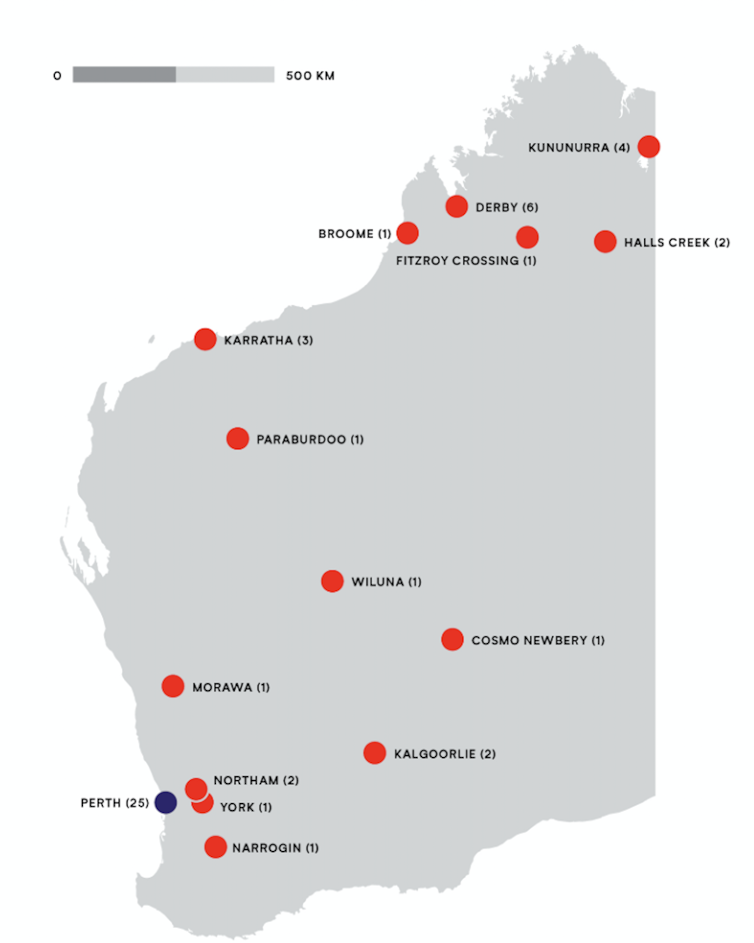
Over two years, we recruited 38 native patients and 52 eyes (some patients had DMO in each eyes). Patients were recruited from each Perth and Western Australia. At enrollment, they were randomly assigned to receive a dexamethasone implant or an anti-VEGF agent. I found. Followed up for checkup and retreatment. After 12 months, we analyzed all our data, to match the security and effectiveness of the 2 drugs.
Results Patients who received the dexamethasone implant gained 4 additional letters on the usual eye chart, which equates to a 6.2 percent improvement of their vision. Those who received the anti-VEGF agent, meanwhile, lost a mean of 5.5 letters, representing an 8.9 percent reduction.
Taken together, these results represent a visible gain of 15% (9.5 letters) for patients receiving the dexamethasone implant. In real-world terms, which means that patients make appointments Visual requirements for a private driver's license. Those who received an anti-VEGF agent didn’t.
This disparity was most pronounced in urban areas of the country, where the dexamethasone implant had a 37% (24 letters) advantage over the anti-VEGF agent.
The creator provides.
Why it really works
As we suspected, the higher performance of the dexamethasone implant is said to its less frequent, due to this fact more practical, dosing regimen.
Over 12 months, patients who were scheduled to receive 4 injections of the dexamethasone implant received a mean of three.3 injections. This meant that, on average, they received 82.5 percent of their desired treatment.
Meanwhile, anti-VEGF patients received 7.2 of their scheduled 12 injections. This equates to only 60% of their required treatment, and reflects the problem of attending monthly appointments in the actual world. Anti-VEGF patients had twice as many injections as dexamethasone implant patients, yet had poorer vision.
Not all results were positive. One-third of patients who received a dexamethasone implant developed increased intraocular pressure – a recognized side effect of steroid injections. While not painful, prevention requires treatment with pressure-reducing drops and shut follow-up. Glaucoma.
Secondly, the speed of steroid injection is quicker. Cataract Formation (clouding of the lens in the attention). This requires access to cataract surgery, which isn’t at all times easy to rearrange in distant locations. Based on these caveats, we developed guidelines for the judicious use of dexamethasone implants in indigenous patients. Published in March..
Reducing the load, closing the vision gap
While dexamethasone implants will not be perfect, we consider the OASIS study offers hope for reducing the “treatment burden” for Indigenous Australians with vision loss and diabetes.
The ability to conduct culturally secure clinical trials signifies that latest treatments may be evaluated in the identical way in the longer term, taking input from patients under consideration. Community controlled research.














Leave a Reply