While Sophie was pregnant together with her first child, she had a baby boy. Oral glucose tolerance Blood tests. A number of days later, the hospital called to inform her she had gestational diabetes.
Despite the slight rise in glucose (blood sugar) levels, Sophie describes her diagnosis as having a big impact on her pregnancy. She checked her blood glucose levels 4 times a day, kept a food diary and made additional appointments with doctors and nutritionists.
Due to the danger of getting a big baby, she was advised to undergo an induction. At 39 weeks, her son was born, weighing a median of three.5 kg. But he was avoided the couch for 4 hours to watch his glucose levels.
Sophie just isn’t alone. with reference to One in six Pregnant women in Australia at the moment are diagnosed with gestational diabetes.
It wasn't at all times like that. The new standard was developed in 2010 that omitted the initial screening test and lowered the diagnostic set points. Gestational diabetes has since been diagnosed. More than double.
AIHW, The creator provides.
But Recent the study Call into query the best way we diagnose and manage gestational diabetes, especially for ladies like Sophie who’ve mild glucose tolerance. Here's What's Wrong With Gestational Diabetes Screening
Glucose tests are unreliable.
The test used to diagnose gestational diabetes – the oral glucose tolerance test – has low reproducibility. This signifies that subsequent tests may give different results.
In a ___ A recent Australian trial In early pregnancy tests, one-third of ladies initially classified as having gestational diabetes (but neither told nor treated) were found to have gestational diabetes when retested after pregnancy. was not This is an issue.
Usually when a test has poor reproducibility – for instance, blood pressure or cholesterol – we repeat the test to substantiate before making a diagnosis.
Most of the rise within the incidence of gestational diabetes following the introduction of the brand new diagnostic criteria was as a consequence of the shift from using two tests to using just one test for diagnosis.

Shutterstock
The limits are very low.
Despite little evidence of profit for either women or children, the present Australian criteria only diagnose women with mild to abnormal outcomes as “gestational diabetes”.
Recent studies show that it doesn’t profit women and will harm them. Oh The New Zealand trial Over 4,000 women were randomly assigned to be tested based on the present Australian threshold or higher threshold level (much like pre-2010 criteria).
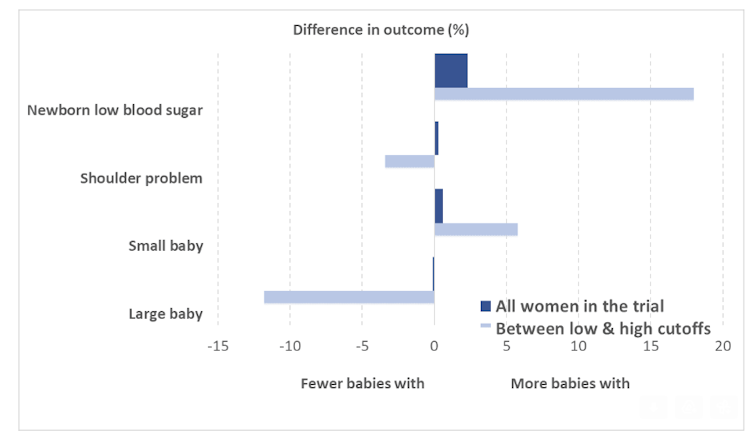
Using the present lower cut-off level within the trial showed no additional profit, with no overall difference within the proportion of babies born large for gestational age.
However, the trial found several harms, including higher neonatal hypoglycemia (low blood sugar in newborns), labour, use of diabetes medications including insulin injections, and use of health services.
The study authors also checked out the subgroup of ladies who were diagnosed with glucose levels between the high and low thresholds. In this subgroup, there was some reduction in older children, and shoulder problems at birth.
But there was also a rise in young children. This is worrisome because being small for gestational age can have consequences for babies as well, including long-term health consequences.
NEJM, The creator provides.
Testing very soon
Some centers have begun screening women at high risk for gestational diabetes early in pregnancy (between 12 and 20 weeks).
However, one A recent trial Tests at 24-28 weeks typically showed no clear advantage: possibly fewer older babies, but again more much like younger babies.
There was a discount in transient “respiratory distress” – requiring supplemental oxygen for a couple of hours – but not in serious medical events.
Effects on women with gestational diabetes
For women with high glucose tolerance, dietary advice, glucose monitoring and, where vital, insulin therapy reduce complications during delivery and the postpartum period.
However, current models of care also can cause harm. Women with gestational diabetes are sometimes denied their preferred model of care – for instance, midwifery continuity of care. In rural areas, they could must be transferred to a bigger hospital, which requires long trips for prenatal visits, and to a bigger center for his or her births – leaving their families and support behind. Away from networks for several weeks.
Women say the diagnosis often dominates their prenatal care and their entire lives. Pregnancy experienceFreeing up time for other issues or concerns.
Women from culturally and linguistically diverse communities Find the difficulty Adapting advice about food regimen and exercise to their very own cultural practices and beliefs about pregnancy.
Some women who’ve gestational diabetes. become Are extremely concerned about their food and adopt extensive calorie restrictions or poor eating habits.

Unsplash/Jordan Bauer
Time to reassess the recommendation
Recent evidence from each randomized controlled trials and qualitative studies with women diagnosed with gestational diabetes suggests that we want to re-evaluate how we currently diagnose and manage gestational diabetes. Especially for ladies with barely higher levels.
It is time to review considering all the problems mentioned above. This review should include the views of all those affected by these decisions: women of their childbearing years, and the GPs, dieticians, diabetologists, midwives and obstetricians who take care of them.














Leave a Reply